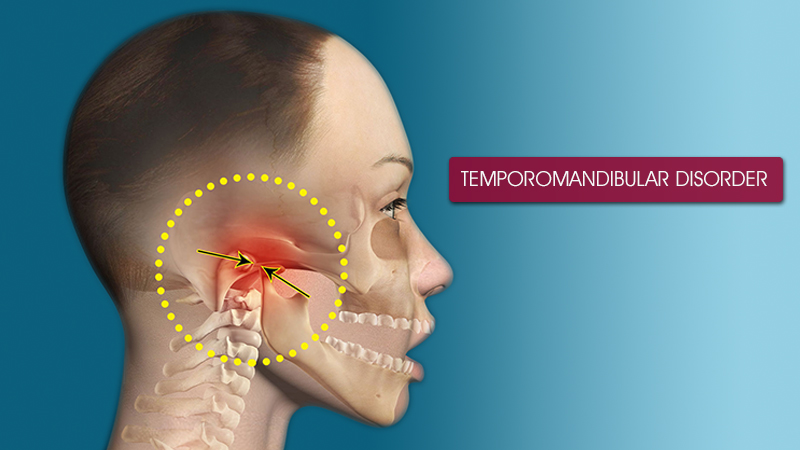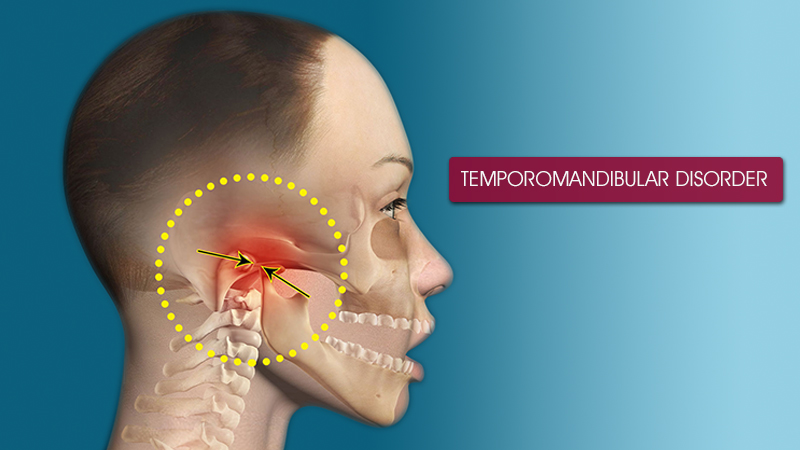
Temporomandibular joint disorder in noida (TMJD or TMD), or TMJ syndrome, is an umbrella term covering acute or chronic inflammation of the temporomandibular joint, which connects the mandible to the skull. The disorder and resultant dysfunction can result in significant pain and impairment. Because the disorder transcends the boundaries between several health-care disciplines - in particular, dentistry and neurology - there are a variety of treatment approaches.
The temporomandibular joint is susceptible to many of the conditions that affect other joints in the body, including ankylosis, arthritis, trauma, dislocations, developmental anomalies, and neoplasia.
An older name for the condition is "Costen's syndrome", after James B. Costen, who partially characterized it in 1934
Signs and symptoms of temporomandibular joint disorder vary in their presentation and can be very complex, but are often simple. On average the symptoms will involve more than one of the numerous TMJ components: muscles, nerves, tendons, ligaments, bones, connective tissue, and the teeth. Ear pain associated with the swelling of proximal tissue is a symptom of temporomandibular joint disorder.
Symptoms associated with TMJ disorders may be:
- Biting or chewing difficulty or discomfort
- Clicking, popping, or grating sound when opening or closing the mouth
- Dull, aching pain in the face
- Earache (particularly in the morning)
- Headache (particularly in the morning)
- Hearing loss
- Jaw pain or tenderness of the jaw
- Reduced ability to open or close the mouth
- Tinnitus
- Neck and shoulder pain
- Dizziness Contents
Unlike a typical finger or vertebral junctions, each TMJ actually has two joints, which allows it to rotate and to translate (slide). With use, it is common to see wear of both the bone and cartilage components of the joint. Clicking is common, as are popping and deviations in the movements of the joint. Pain is the most conventional signifier of TMD.
The surfaces in contact with one another (bone and cartilage) do not have any receptors to transmit the feeling of pain. The pain therefore originates from one of the surrounding soft tissues, or from the trigeminal nerve itself, which runs through the joint area. When receptors from one of these areas are triggered, the pain can cause a reflex to limit the mandible's movement. Furthermore, inflammation of the joints or damage to the trigeminal nerve can cause constant pain, even without movement of the jaw.
Due to the proximity of the ear to the temporomandibular joint, TMJ pain can often be confused with ear pain.[6] The pain may be referred in around half of all patients and experienced as otalgia (earache).[7][8] Conversely, TMD is an important possible cause of secondary otalgia. Treatment of TMD may then significantly reduce symptoms of otalgia and tinnitus, as well as atypical facial pain. Despite some of these findings, some researchers question whether TMD therapy can reduce symptoms in the ear, and there is currently an ongoing debate to settle the controversy.
The dysfunction involved is most often in regards to the relationship between the condyle of the mandible and the disc. The sounds produced by this dysfunction are usually described as a "click" or a "pop" when a single sound is heard and as "crepitation" or "crepitus" when there are multiple, rough sounds.
Disorders of the teeth can contribute to TMJ dysfunction.[14] Impaired tooth mobility and tooth loss can be caused by destruction of the supporting bone and by heavy forces being placed on teeth. The movement of the teeth affects how they contact one another when the mouth closes, and the overall relationship between the teeth, muscles, and joints can be altered. Pulpitis, inflammation of the dental pulp, is another symptom that may result from excessive surface erosion. Maybe the most important factor is the way the teeth meet together: the equilibration of forces of mastication and therefore the displacements of the condyle. Many report TMJ dysfunction after having their wisdom teeth extracted.